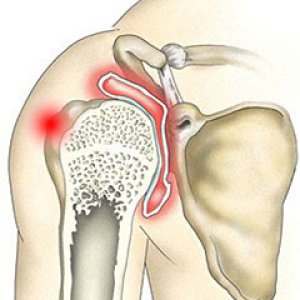
Although most people think of the shoulder as multiple joints, there are actually two joints in the shoulder area. One is located where the clavicle (collar bone) meets the tip of the shoulder bone (acromion). This is called the acromioclavicular joint or AC joint.
The junction of the upper arm bone (humerus) with the scapula (shoulder blade) is called the glenohumeral joint or scapulothoracic joint. Both joints can be affected by arthritis. To provide you with effective treatment, your doctor will have to determine which joint is affected and what type of arthritis you have.