After alternative measures have been exhausted, surgical intervention may be necessary in circumstances of exacerbated pain or neurological deficits. In spite of good therapeutic results from conventional operations, consecutive damage may result from traumatization. Therefore, it is important to optimize the spine procedures. The aim in this process of continuous improvement is to minimize the trauma induced by the operation and negative long-term effects while observing existing quality standards.
Spine

Full Endoscopic Decompression Spine

Minimally invasive techniques allow tissue damage and its consequences to be reduced. Endoscopic operations carried out during a continuous flow of fluid demonstrate advantages which these procedures standard practice in many areas.
After alternative measures have been exhausted, surgical intervention may be necessary in circumstances of exacerbated pain or neurological deficits. In spite of good therapeutic results from conventional operations, consecutive damage may result from traumatization. Therefore, it is important to optimize the spine procedures. The aim in this process of continuous improvement is to minimize the trauma induced by the operation and negative long-term effects while observing existing quality standards.
Minimally invasive techniques allow tissue damage and its consequences to be reduced. Endoscopic operations carried out during a continuous flow of fluid demonstrate advantages which these procedures standard practice in many areas.



Full endoscopic surgery on the cervical, thoracic, and lumbar spine provides and adequate and safe complement or alternative to conventional surgery. A change is taking place for the first time as a result of the latest technical developments and new access passages, which appears to be the start of a radical new departure comparable with the establishment of arthroscopic procedures in joints.
The development of full endoscopic methods should not be evaluated as a replacement of existing standard operations but as complimentary procedure and alternative within the overall concept of spine surgery.






Full endoscopic surgery on the cervical, thoracic, and lumbar spine provides and adequate and safe complement or alternative to conventional surgery. A change is taking place for the first time as a result of the latest technical developments and new access passages, which appears to be the start of a radical new departure comparable with the establishment of arthroscopic procedures in joints.
The development of full endoscopic methods should not be evaluated as a replacement of existing standard operations but as complimentary procedure and alternative within the overall concept of spine surgery.
Lateral Transforaminal Access


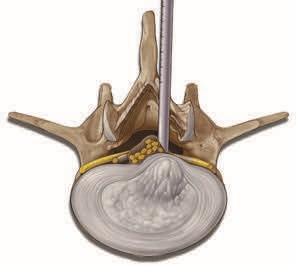
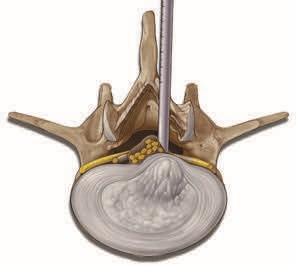
At the start of the spinal canal, the spinal cannula contacts the posterior annulus in the medial pedicle line. Insertion of the dilator along the guide wire until the spinal canal or posterior annulus defect. The endoscope is inserted through the working sleeve. The lateral access permits working the spinal.






Posterolateral Access




Operation with posterolateral transforaminal access has the entry point in the skin is determined by the Pathology and anatomy, and can be measured in Centimeters from the midline.
Transforaminal and Extraforaminal Access






In the case of intraforaminal and extraforaminal spinal disk hernia- tions and foraminal stenoses, there may be an increased risk of injury to the exiting nerves during the passage through the foramen with the access instrument set. The extra- foraminal access may be necessary here. The entry point into the skin is possible from posterolateral to lateral. The spinal cannula is not guided through the foramen into the spinal canal but on the caudal pedicle of the level to be operated.
This is the safest zone in relation to the exiting nerves and an access-related risk is avoided. The guide wire, dilator and operating sleeve are then also inserted on to the pedicle up to the bony contact. The anatomical structures of the caudal foramen and the exiting nerve can then be dissected in vision and the surgical intervention can be carried out with conservation of the nerves.
Full-Endoscopic Interlaminar Access




Direct access to the epidural space with continuous visualization is hence necessary for adequate operations within the spinal canal. Lateral access is necessary for this when using the full-endoscopic transforaminal technique. The bony and neural boundaries of the neuro- foramen define limits for mobility and hence also in relation to the indication criteria. Furthermore, the necessary lateral access in the lower levels may be prevented by the pelvis. On the basis of our experience, these restrictions encompass a spectrum of pathologies which are not operable using the full-endoscopic transforaminal approach due to technical limitations.



Direct access to the epidural space with continuous visualization is hence necessary for adequate operations within the spinal canal. Lateral access is necessary for this when using the full-endoscopic transforaminal technique. The bony and neural boundaries of the neuro- foramen define limits for mobility and hence also in relation to the indication criteria. Furthermore, the necessary lateral access in the lower levels may be prevented by the pelvis. On the basis of our experience, these restrictions encompass a spectrum of pathologies which are not operable using the full-endoscopic transforaminal approach due to technical limitations.






Making use of anatomically preformed access areas is effective for reducing surgically related traumatization to the structures of the spinal canal. Alongside the inter- vertebral foramen, the sacral hiatus and the interlaminar window are located here. Resection of large pathologies is not possible in technical terms using epiduroscopy through the sacral hiatus. The surgical access through the interlaminar window is therefore used. This has been familiar in lumbar spine surgery for the longest and is frequently used. It has been described since the beginning of the 1920s. Alternative methods were subsequently developed, such as the posterolateral approach for taking biopsies from vertebras at the end of the 1940s or intra- diskal decompression using chemonucleolysis in the early 1970s. Endoscopic inspections of the intervertebral space after open decompression were described during the early 1980s. The implementation of full-endoscopic operations concentrated on the transforaminal technique with postero- lateral access.
Making use of anatomically preformed access areas is effective for reducing surgically related traumatization to the structures of the spinal canal. Alongside the inter- vertebral foramen, the sacral hiatus and the interlaminar window are located here. Resection of large pathologies is not possible in technical terms using epiduroscopy through the sacral hiatus. The surgical access through the interlaminar window is therefore used. This has been familiar in lumbar spine surgery for the longest and is frequently used. It has been described since the beginning of the 1920s. Alternative methods were subsequently developed, such as the posterolateral approach for taking biopsies from vertebras at the end of the 1940s or intra- diskal decompression using chemonucleolysis in the early 1970s. Endoscopic inspections of the intervertebral space after open decompression were described during the early 1980s. The implementation of full-endoscopic operations concentrated on the transforaminal technique with postero- lateral access.



Since the end of the 1970s, the microsurgical procedure using the microscope has also been developed and today this has achieved the status of “Gold Standard” for inter- laminar decompression in the area of the spinal canal. Details of an endoscopically assisted technique known as a microendoscopic operation were published in the late 1990s. This relates to visualization of the opened operation site using an endoscope and a monitor.



Since the end of the 1970s, the microsurgical procedure using the microscope has also been developed and today this has achieved the status of “Gold Standard” for inter- laminar decompression in the area of the spinal canal. Details of an endoscopically assisted technique known as a microendoscopic operation were published in the late 1990s. This relates to visualization of the opened operation site using an endoscope and a monitor.



Opening the spinal canal is necessary in the conventional method for reaching the epidural space. This generally involves incision of the ligamentum flavum and resection of bone. Adequate access must be created which ensures vision into the spinal canal and permits working with instruments. Problems may arise as a result of trauma- tization of the access passage, as a result of resection of stabilizing structures and in particular in relation to potential revisions resulting from scar formation. The microscope principally reduces the size of the access passage and creates very good light and envisioning conditions.
